Navigating life with Postural Orthostatic Tachycardia Syndrome (POTS), hypermobility, or Ehlers-Danlos Syndrome (EDS) presents unique challenges, especially in the realm of exercise. While exercise is important for overall health and is part of the rehabilitation process, the traditional approach to exercise may not always be suitable for individuals with chronic health conditions. Utilising a personalised approach that acknowledges and adapts to the individual is crucial to long-term success. In this blog, we will delve into how exercise can be personalised to your needs. We will also discuss how to understand and apply the Rate of Perceived Exertion (RPE) Scale to your activities to help find appropriate levels of exercise intensity.
Foundations for a Personalised Approach
Successfully managing POTS, hypermobility, and EDS through exercise incorporates cardiovascular exercise in combination with strength training. You may have heard of or been recommended to complete the Levine or Dallas/CHOP Protocols for POTS rehab; these protocols were adapted from the training methods used in POTS research studies. Based on research the gold standard is to do 3-4 days of cardio and 2 days of strength exercises.
They typically are set out in the following phases:
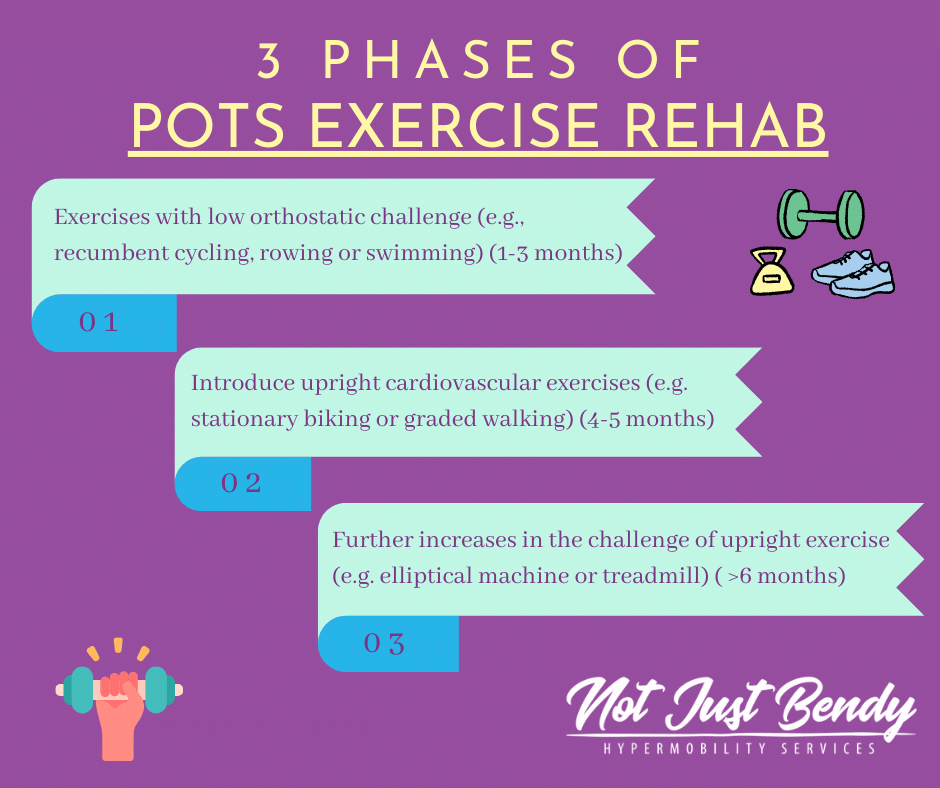
- Phase 1 (1-3 months): Exercises with low orthostatic challenge such as recumbent cycling, rowing ergometer or swimming
- Phase 2 (4-5 months): Introduces upright cardiovascular exercises such as stationary biking and graded walking, as your body starts to adapt.
- Phase 3 (6 months and beyond): Further increases the challenge of upright exercise, including the elliptical machine and treadmill.
Fatigue, pain, and associated symptoms of ME/CFS (chronic fatigue syndrome), can be a barrier to even getting started and meeting the frequencies recommended. Fatigue is also the main reason for participant drop out in research studies.
Using the basis of these research protocols and considering your individual situation is how ‘Not Just Bendy’ physiotherapists and exercise physiologists can help you come up with a personalised exercise program that you can tolerate.
Making Exercise Work for You
Exercise is not one-size-fits-all, especially for those with chronic health conditions. Each person’s experience with POTS and hypermobility varies, and factors such as current symptoms, energy levels, and coexisting conditions must be considered when developing a program. What works for one person may not work for another.
Many people associate exercise with intense workouts that leave them feeling exhausted and out of breath. A big part of our education with clients is reframing this and understanding that exercise doesn’t have to be hard and exhausting to be beneficial. Even short bouts of light activity can have positive effects.
When energy levels and pain are a barrier to exercise, it’s essential to listen to your body and adjust your exercise routine accordingly. This may mean modifying the type, intensity, and duration of exercise based on how you’re feeling that day. Pacing, avoiding boom and bust cycles and consistency are key. Remember that progress may not always be linear, and it’s okay to experience setbacks. Life changes, increased stress or illness, may necessitate adjustments to your exercise routine. Having an adaptable program ensures that exercise remains a sustainable and enjoyable part of your lifestyle.
Below we will share two stories of client programs based on the above principals and how we at Not Just Bendy are able to tailor POTS rehabs to those with varying severity of POTS and symptomatic hypermobility/EDS.
Margret’s Story:
Margret* is in her mid-40’s and has both H-EDS, POTS and MCAS (Mast Cell Activation Syndrome). Margret works full-time and is a busy parent. She has been active all her life however always found cardiovascular exercise particularly challenging; her HR would get high very quickly and would feel faint and dizzy after an extended period. In recent years, Margret was diagnosed with POTS and takes a heart lowering medication for management. Currently, she attends a group exercise class 2-times a week to focus on global muscle strengthening and completes a small home program for joint-specific issues but did not find that her POTS and fatigue were improving.
As part of her program updated through Not Just Bendy she has included POTS specific cardiovascular exercises, and has now progressed to an upright, interval-based program. The base program is done on an upright bike with a 5-10mins warm up, followed by 5-rounds of 45sec higher intensity intervals and 2mins active rest, then finishing with a 5-10min warm up. Margret was taught to self-adjusts this program depending on how her body is feeling each day. Due to various external factors such as fatigue and stress she may is not able to tolerate a full 5-rounds of intervals, on those days she will do a shorter session. Margret’s gym can be quite warm and she is not always able to tolerate upright exercises, so she follows the same program on a recumbent bike. The current progression plan for Margret is to work on decreasing her rest periods with her interval training. Margaret now feels more energised after the gym (instead of drained) and has spoons left to complete her daily tasks easily.
Charlotte’s Story:
On the other flipside we have Charlotte* who is in her late 20’s with generalised-joint hypermobility, ME/CFS and POTS. Charlotte has been unwell the past few years with pain and fatigue being major limiters to her day-to-day function. As such she was often bedbound and deconditioned when she first attended Not Just Bendy.
Her initial program and sessions involved education on symptom management and pacing. All her rehab exercises are down laying down focusing on improving joint stability and isometric strength exercises for the leg muscles. She has been working on slowly increasing her upright tolerance by increasing sitting time and take a walk around the house when able. Six months in, we have now been able to introduce gentle seated stationary pedal exercises working starting once a week for 5mins at a constant pace, low intensity, and building towards increasing her exercise duration. Charlotte has much improved tolerance for short walks around her home and has ventured to the local coffee shop with a friend in her wheelchair which has been a goal for a few years.
The RPE Scale Explained
The RPE scale ranges from 1 to 10. It provides a subjective rating of how intense an exercise feels. The scoring is completely individualised to each person and is variable over time. It is a simple measure that does not depend on other metrics such as speed, weight, or heart rate (which is not always reliable for those on heart rate-lowering medication for POTS). We can use this simple measure to adjust exercise intensities accordingly to your needs.
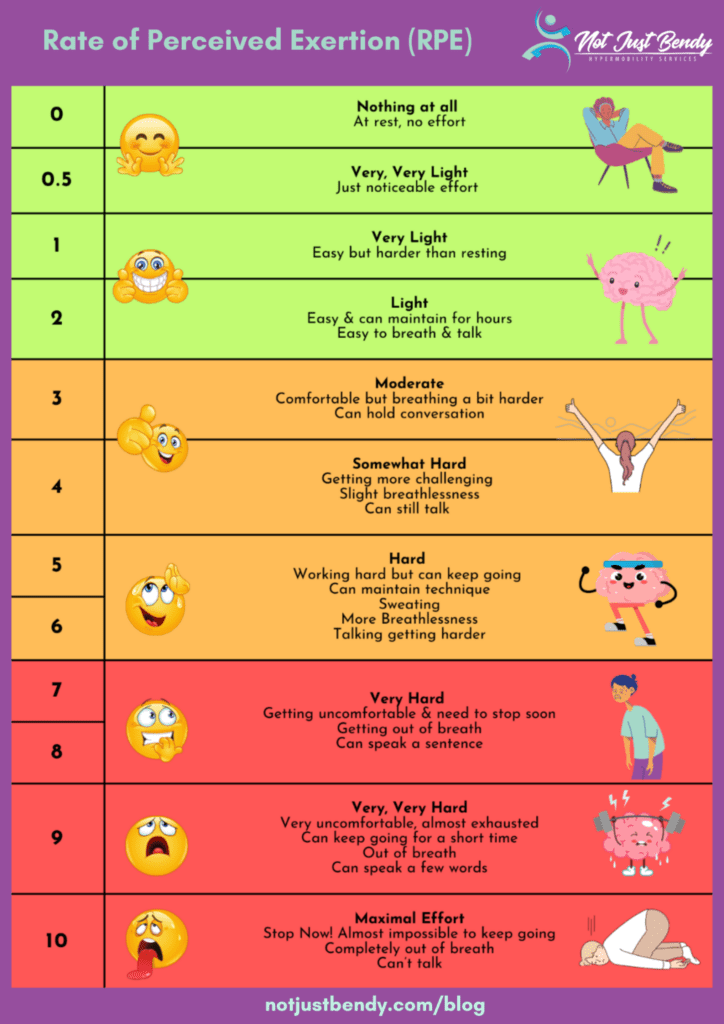
The RPE Scale:
- 1-2: These levels indicate very light activity. You should be able to converse easily without any breathlessness.
- 3-4: Activities falling into this category are considered moderate. You might notice your breathing rate increase, but you’re not out of breath.
- 5-6: Here, you’re entering a zone that’s challenging yet still manageable. Conversation becomes harder, signalling increasing cardiovascular effort.
- 7-10: These levels represent high to maximum effort. Speaking is very difficult due to the intensity of the exercise, indicating that you’re pushing the limits of your capacity. Activities in these zones are not intended to be sustained for long periods.
Applying RPE in Your Exercise Program
As mentioned earlier RPE is personalised and variable over time. It allows for day-to-day adjustments based on how you feel, ensuring that you’re exercising within an appropriate and beneficial intensity range for each given day.
- Starting Low: Begin with exercises that are low on the RPE scale, particularly if you’re new to exercising. This might include activities like your rehab program, mobility exercises, gentle swimming or recumbent cycling.
- Monitoring Progress: As you become more comfortable, gradually increase the intensity of workouts such gentle walking, upright cycling and progressed strength exercises to higher RPE ranges. As you become more aware of your body and how it responds to exercise, you can also use RPE to help keep your day-to-day activities within a range that does not cause further fatigue and pain flare ups-post.
- Adjusting for Symptoms: On days where symptoms are more pronounced your RPE may not always be at ‘0’ when resting, on those days you may only have the capacity to increase you RPE a little during exercise a little or are better to rest instead.
Exercising with POTS – Tips for Success
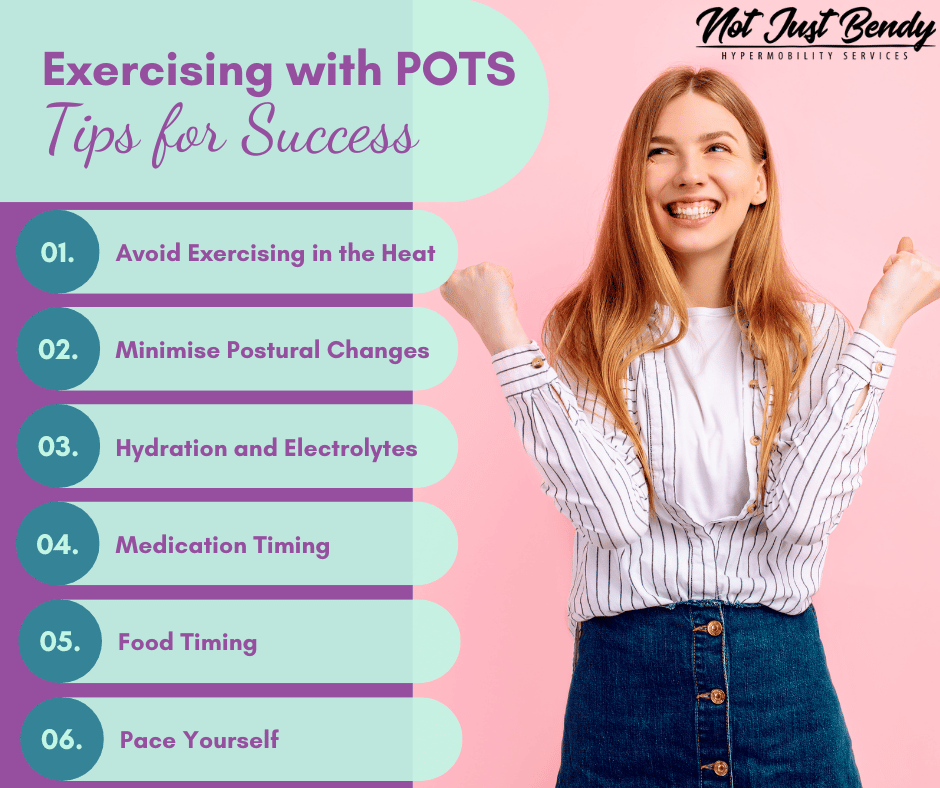
- Avoid Exercising in the Heat – Exercising in hot conditions can worsen POTS symptoms.
2. Minimize Postural Changes – Plan workouts to limit the need for frequent changes in posture, reducing the strain on your cardiovascular system.
3. Hydration and Electrolytes – Consuming fluids and electrolytes 20-30 minutes before working out helps expand blood volume, potentially reducing exercise-induced symptoms. Keep hydrated throughout your session to maintain blood volume.
4. Medication Timing – Timing exercise with the peak effectiveness of your medication can improve exercise tolerance and reduce symptoms whilst exercising.
5. Food Timing – Avoid eating 2 hours before exercising to minimize gastrointestinal discomfort and reduce blood flow diversion to the intestines for digestion.
6. Pace Yourself – It’s crucial to progress at your own pace. Active recovery and rest are just as important as progression, ensuring that every step forward is sustainable.
Exercise, when appropriately tailored is a powerful tool for those living with POTS, hypermobility, and EDS. Your body’s responses, your progression pace, and your collaboration with your practitioner are the foundations to a successful program. Each person will progress through each ‘Phase’ at their own pace. By utilising a personalised approach to exercise, “Not Just Bendy Hypermobility Services” is committed to supporting you every step of the way in your journey.
Referral to Our Exercise Physiologist and Physiotherapists for POTS management
If you’re looking for personalized support and guidance in managing POTS, hypermobility, or EDS through exercise, our in-house exercise physiologist, Avery, is here to help. Avery specialises in creating tailored exercise programs that cater to your unique needs and health conditions. Additionally, we have a team of skilled physiotherapists who are experienced in working with individuals with hypermobility and EDS. To learn more about our services or to schedule a consultation, please visit our website and explore our team of professionals. Let us support you on your hypermobility journey.

References:
- Fu, Q., & Levine, B. D. (2015). Exercise in the postural orthostatic tachycardia syndrome. Autonomic neuroscience : basic & clinical, 188, 86–89. https://doi.org/10.1016/j.autneu.2014.11.008
- Fu, Q., & Levine, B. D. (2018). Exercise and non-pharmacological treatment of POTS. Autonomic neuroscience : basic & clinical, 215, 20–27. https://doi.org/10.1016/j.autneu.2018.07.001
- Shibata S, Fu Q, Bivens TB, Hastings JL, Wang W, Levine BD. Short-term exercise training improves the cardiovascular response to exercise in the postural orthostatic tachycardia syndrome. J Physiol. 2012 Aug 1;590(15):3495-505. doi: 10.1113/jphysiol.2012.233858. Epub 2012 May 28. PMID: 22641777; PMCID: PMC3547265.
- Instructions for POTS Exercise Program—Children’s Hospital of Philadelphia (CHOP) Protocol

Want To Learn More From Sharon Hennessey About Hypermobility?
Sharon’s ground-breaking hypermobility educational courses are launching soon – sign up now to know when the courses go live!
Join the wait list to be the first to access exclusive video content, tailored for health professionals, patients, carers, and anyone seeking to better understand hypermobility.
