Understanding Hypermobile Hips: Causes and Treatments
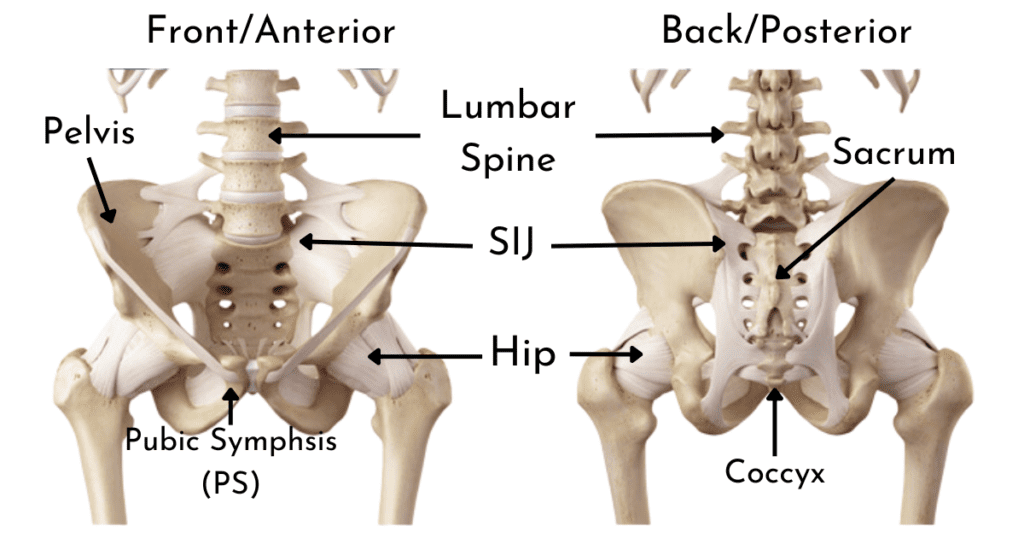
As a physiotherapist in Brisbane, Australia, with a special interest in hypermobility-related connective tissue disorders, I primarily work with clients who have hypermobile Ehlers-Danlos Syndrome (hEDS), Hypermobility Spectrum Disorder (HSD), or Asymptomatic Generalised Hypermobility. Over the years, I have observed that approximately 90% of symptomatic hypermobility clients experience issues involving the hips or pelvis. Common complaints include sensations of locking, giving way, clunking, popping, incontinence, and pain. These problems can arise from several structures, including the joints (hip, sacroiliac joint (SIJ), and pubic symphysis), soft tissues (muscles and tendons), nerves, or referred pain from the lower back and surrounding areas.
Given that hypermobile individuals often suffer from pain and instability across multiple regions of the body, it is not surprising that the hips and pelvis are frequently involved. However, in my experience, targeted rehabilitation focused on the hips, pelvis, and low back can be critical in enhancing quality of life. Effective rehabilitation in these areas helps maintain or restore function, regardless of whether a client presents with mild or complex hypermobility symptoms.
“The hip joint is often an enigma to many physical therapists, but with targeted rehabilitation programs, improved hip control and alignment can not only improve hip symptoms but also other issues throughout the body for those with symptomatic hypermobility.” – Sharon Hennessey
Why are the Hips and Pelvis so Important in the Rehabilitation of a Hypermobile Individual?
The hip and pelvis area plays a vital role in providing stability and balance throughout the body, making it essential for several reasons:
- Support and Protection of Vital Organs: The pelvis acts as a protective structure for organs such as the bladder, uterus, bowel, and intestines. Ensuring stability in this area can support the proper function of these organs.
- Pelvic Floor Function: The muscles of the pelvic floor control bladder and bowel function. Weakness in these muscles can result in stress incontinence, while overactivity can lead to an overactive bladder, constipation, and even painful intercourse.
- Joint Proprioception: The muscles surrounding the hip joint provide critical sensory information to the brain about body position, helping coordinate balance and movement. This is particularly important for hypermobile individuals, in whom proprioception can be impaired.
- Gluteus Maximus Strength: The gluteus maximus, the largest muscle in the body, is essential for everyday movements such as standing from a seated position, walking uphill or upstairs, and squatting. Its strength is fundamental to maintaining mobility and independence.
- Stabilising Muscles: The deeper stabilising muscles of the hip and pelvis, including the deep hip flexors, gluteus minimus, and the deep external rotators, play a crucial role in providing a sense of stability to the hip joint. Rehabilitation can help reduce unwanted clunks, pops, and cracking sensations through proper muscle engagement and timing.
- Efficient Movement: Transferring weight from one leg to the other during walking requires coordination of the hip and pelvis. Poor control in this area often results in inefficient movement, which can lead to compensatory problems and additional pain.
- Postural Base: The hip and pelvis form a stable postural base that supports upper body function during walking and standing. Imbalances here can affect areas like the neck, shoulders, and knees, leading to widespread discomfort.
- Trendelenburg Gait and Hip Drop: A noticeable “hip drop,” or Trendelenburg gait, is often linked with painful conditions like gluteal tendinopathy, SIJ issues, and knee or foot problems. Improving control around the pelvis can help address these movement patterns.
- Chronic Ankle Sprains and Hip Muscle Wastage: Research indicates that those with a history of ankle sprains may have reduced lateral hip muscle strength. Since many hypermobile individuals experience chronic ankle instability, strengthening the entire lower limb, particularly the lateral hip, is important for overall stability and function.
- Muscle Overactivity Relief: Improved control of the hip muscles can often relieve overactivity in other muscles, such as those in the thoracic (middle back) and lumbar (lower back) regions. By targeting hip rehabilitation, individuals can experience less pain and muscle gripping elsewhere in the body.

Effective Muscle Coordination and Timing
One of the key aspects of rehabilitation is the coordination and timing of muscle activity, not just strength. The ability to transfer your weight smoothly and effectively from one leg to the other while walking requires the synchronized action of many muscles. It’s essential to retrain the brain to activate the appropriate muscle at the right time and intensity. This is particularly relevant for hypermobile individuals, in whom muscle recruitment patterns may be altered.
Building strength alone is not sufficient. In fact, overworking a single muscle or muscle group can place undue stress on other areas. That’s why muscle timing – the coordination of muscle activation, is so important. Strategies to manage muscle tightness and overactivity should also be implemented carefully. In many hypermobile clients, muscle tension may actually be compensating for underlying instability. As such, strength and stability must be built before focusing on releasing these compensatory tensions.
Research: Hypermobile Disorders and the Hip Joint
Recent research has shed light on the effects of hypermobile disorders on the hip joint, offering valuable insights into the management of these conditions. According to a 2021 article by Clapp et al. titled “Hypermobile Disorders and Their Effects on the Hip Joint,” several important findings stand out:
- Increased Incidence of FAIS (Femoroacetabular Impingement Syndrome): Individuals with hypermobility are more susceptible to conditions like FAIS, premature arthritis, and capsular degeneration. These conditions can significantly impact the stability and function of the hip joint, resulting in pain and dysfunction.
- Individualised Physiotherapy Management: The study emphasises the importance of tailoring physiotherapy management to each individual. Strengthening the dynamic muscles surrounding the hip is crucial to enhance stability, particularly in hypermobile clients. Given the unique challenges posed by hypermobility, a one-size-fits-all approach ineffective; therapy must focus on addressing both muscle strength and timing deficits.
- Capsular Management in Surgery: For hypermobile clients requiring surgical intervention, careful attention to capsular management is essential. Techniques such as capsular plication or capsular shift can increase the success of surgery and help prevent postoperative instability. This consideration is particularly important, as hypermobile individuals may be more prone to postoperative instability.
- The Impact of Repetitive Micro-Trauma: Repetitive micro-trauma from excessive hip motion is a common issue in hypermobile individuals and often leads to pain and hip joint unsteadiness. This unsteadiness may result from bony deficiencies and/or soft-tissue damage or loss. Strengthening the hip musculature and modifying activities are key strategies for managing these conditions, as highlighted by Safran (2019).
- Repetitive motions in extreme ranges of motion can result in compensatory soft tissue laxity which further destabilises the hip joint.
- Subluxation in extreme motions: Research by Kolo et al. (2013) found a significant correlation between subluxation and impingement in ballet dancers. Hypermobile individuals, especially those involved in activities requiring extreme hip positions, are at higher risk for posterior subluxation when assuming positions associated with FAIS. This emphasizes the importance of proper rehabilitation and activity modification in hypermobile individuals.
Overall, these findings underscore the need for a comprehensive approach to managing hip issues in hypermobile individuals, with a focus on joint stability and individualised care through both conservative and surgical options.
Things to Avoid When Managing Hip and Pelvic Issues in Hypermobile Individuals
While adopting the right management strategies is essential, it’s equally important to minimise certain activities and behaviours that could worsen symptoms. Here are some common pitfalls to avoid:
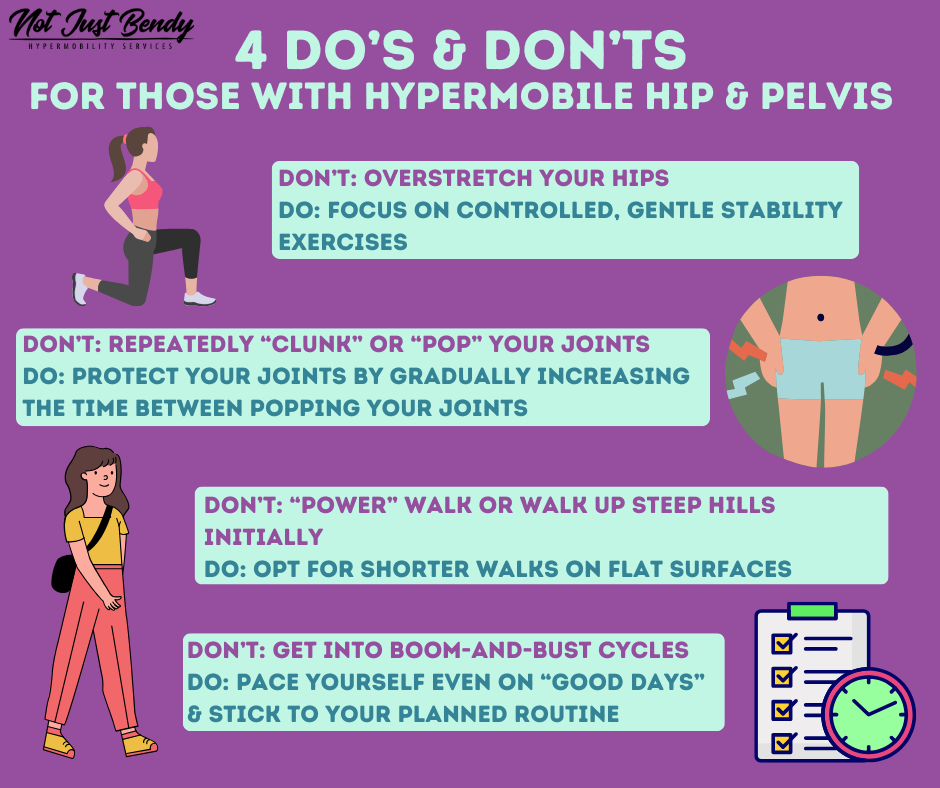
- Overstretching or Forcing Hip Joint Movement: One of the most common mistakes I see in hypermobile individuals is the tendency to overstretch, especially when they feel tightness or discomfort. Although stretching can feel like it’s relieving tension, overstretching can actually be counterproductive, further irritating sensitive areas. It’s important to focus on controlled, gentle movements that prioritise stability over flexibility. Avoid forcing your joints into extreme ranges of motion simply because they can go there —your body needs strength and control, not added looseness.
- Performing Party Tricks or Encouraging Repeated Joint Clunking: It’s not uncommon for hypermobile individuals to feel the need to “clunk” or “pop” their joints into place. While this might offer temporary relief, it often leads to a cycle of needing to repeat the movement more frequently. Next time you feel the need to “clunk” a joint, just try to delay it, gradually increasing the time between these movements. Similarly, performing party tricks that showcase your hypermobility – such as bending your limbs into extreme positions – might seem fun but does no favours for your body in the long run. Protecting your joints is more important than showing off your flexibility.
- Large, Heavy Walking and Excessive Hills During Times of Increased Pain: While staying active is important, pushing yourself too hard when you’re already in pain can exacerbate symptoms. Activities like long walks or walking up steep hills add additional strain on the hips and pelvis, especially during pain flare-ups. It’s essential to modify your activity levels when experiencing increased pain or instability. Opt for shorter walks on flat surfaces, and allow yourself to rest when needed. This will help prevent further aggravation and give your body the opportunity to recover.
- Not Pacing Yourself: Pacing is crucial for managing hypermobility, especially with hip and pelvic issues. Often, people with hypermobility feel compelled to do as much as possible on their “good days”, believing the need to make the most of feeling well. Unfortunately, this can lead to a “boom-and-bust” cycle, where a productive day is followed by intense pain and fatigue. This boom-and-bust cycle is hard on the body and can set you back in your rehabilitation progress. Instead, aim for steady, consistent activity levels. Even on good days, stick to your planned routine, incorporate rest breaks, and avoid overexertion. Effective pacing helps you maintain balance and prevents flare-ups.
Things to Include in Your Management Plan
In addition to avoiding behaviours that could aggravate symptoms, hypermobile individuals can benefit from incorporating specific strategies to improve hip and pelvic stability. These approaches help build strength, prevent injury, and support long-term joint health:
Improving Posture:
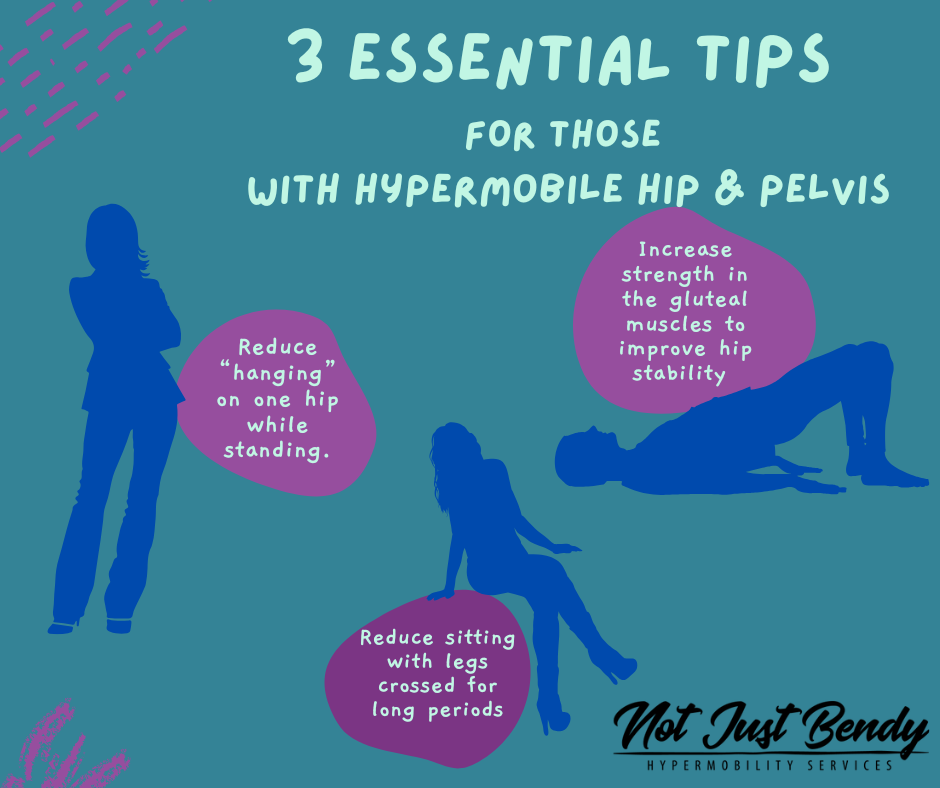
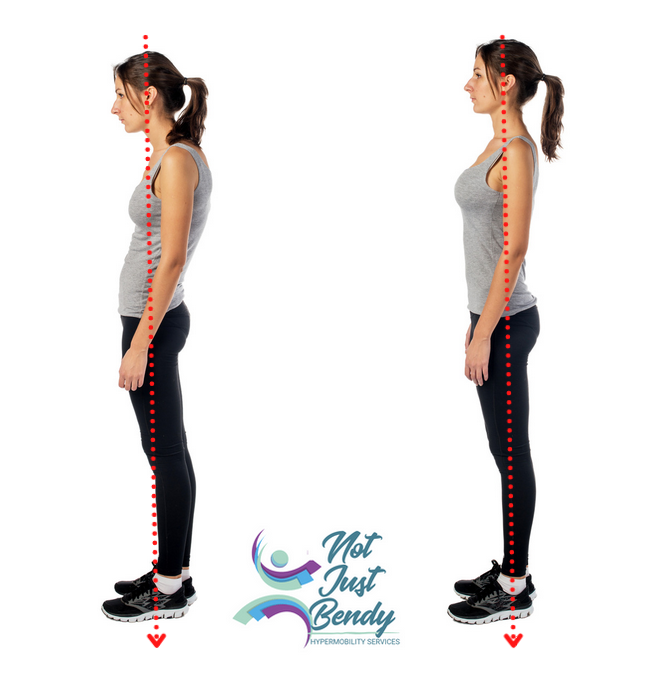
- Avoid Hip Hanging: Many people with hypermobility tend to rely on their joints’ laxity by “hanging” on one hip while standing. This habit may feel comfortable in the moment, but over time place excessive strain on the hip joint, pelvis, and surrounding tissues. To reduce this strain, try to distribute your weight evenly between both legs. You can also try rocking back and forth, shift your weight, or walk on the spot to relieve pressure. When needed, lean on a wall or perch your leg on a stool.


Images: “hanging” on one hip in standing
- Standing with a Large Lordosis (Back Arch): Hypermobile individuals are often prone to standing with an exaggerated arch in their lower back (lordosis). While this might feel like a “natural” posture, it places undue stress on the lumbar spine and pelvis, potentially leading to pain and instability. Instead, focus on bringing your pelvis to rest more evenly on your toes and heels, allowing for a slight, gentle curve in your lower back. Gradually adjust your posture, avoiding holding your breath or tensing your muscles excessively as you make these changes.

- Crossing Legs for Long Periods: Sitting with your legs crossed, particularly for extended durations, places the hips in an asymmetrical position that can lead to muscle imbalances and tension. This posture can exacerbate instability and discomfort, especially for those with hip and pelvic issues. Aim to sit with both feet flat on the floor. If crossing your legs is necessary, try to alternate sides frequently and avoid maintaining the position for too long.
Other Helpful Strategies:
- Sleep with a Pillow Between Your Knees: For side sleepers, placing a pillow between your knees can help maintain your pelvis in a neutral alignment and reduce strain on your hips and lower back. This simple adjustment provides stability during sleep, which is essential for minimizing pain and improving your overall sleep quality. If you sleep on your back, placing a small pillow under your knees can also support a more neutral spine position and alleviate pressure.
- Build Strength in the Gluteal Muscles: The gluteal muscles, particularly the gluteus minimus, medius and maximus, are essential for hip stability. Focus on strengthening these muscles without over-recruiting or tensing the thigh muscles (quadriceps) as overactive quads can create further muscle imbalances. Controlled exercises that isolate the glutes, such as bridges, squats and standing on one leg (without hanging from the hip), can help build gluteal strength while keeping the surrounding muscles relaxed. The goal is to activate the right muscles without overloading others, ensuring balanced strength development.
- Improve Pelvic Control During Single-Leg Stance: One of the most important skills for hip stability is maintaining proper pelvic alignment when standing on one leg. This is crucial to avoid the “Trendelenburg” gait, where the pelvis drops on one side due to weak gluteal muscles. Practice standing on one leg while keeping your pelvis level and engaging your core and gluteal muscles. Use the wall for support on the side of the leg you are lifting and really work on slowly peeling the foot off the ground so that you work on using the muscle of control. Developing strength and control in this position will help stabilise your pelvis during activities like walking, climbing stairs, or any weight-shifting movements.
Management Strategies for Hip and Pelvis Issues in Hypermobile Individuals
Managing hip and pelvic issues in hypermobile individuals requires a combination of targeted therapies, lifestyle adjustments, and, in some cases, surgical intervention.
At Not Just Bendy Hypermobility Services, we understand the unique challenges associated with managing hypermobility and related conditions like hEDS and HSD. Our team focuses on evidence-informed rehabilitation strategies designed to improve stability, reduce pain, and enhance function in hypermobile individuals.
Below are key management strategies that Not Just Bendy can assist you with to help improve your outcomes:
- Strengthening Programs: An individualised strengthening program focused on the dynamic musculature of the hip and pelvis can significantly enhance joint stability. This program should target both large muscle groups like the gluteus maximus and smaller, stabilising muscles such as the deep hip flexors and rotators.
- Proprioception and Coordination Exercises: Rehabilitating the hip requires more than building strength; proprioception and coordination exercises are essential to improve muscle timing and body awareness. These exercises can help retrain the brain to better coordinate muscle activity and maintain balance, contributing to overall stability.
- Activity Modification: For individuals experiencing pain or instability due to extreme ranges of motion, modifying activities may be necessary to avoid repetitive micro-trauma. This could involve adapting exercise routines or altering daily movement patterns to reduce stress on the hip joint.
- Manual Therapy: In some cases, manual therapy techniques like joint mobilisations, soft tissue release, or massage can relief pain and muscle overactivity. However, these therapies should always be paired with a strengthening program to address underlying instability and promote long-term results.
- Surgical Intervention: For those with severe instability or structural damage, surgical options may be necessary. Procedures like capsular plication or capsular shift can help stabilise the hip joint, though careful postoperative rehabilitation is critical to prevent complications.
- Long-term Management: Rehabilitation of the hip and pelvis in hypermobile individuals is often a long-term process. Ongoing strength maintenance, regular assessments, and proactive management of symptoms are essential to preventing relapses and maintaining joint health over time.
- Holistic Management & Advice: Not Just Bendy can help you understand associated co-comorbidities of
References
- Grimaldi A, Mellor R, Hodges P, Bennell K, Wajswelner H, Vicenzino B. Gluteal Tendinopathy: A Review of Mechanisms, Assessment and Management. Sports Med. 2015;45(8):1107‐1119. doi:10.1007/s40279-015-0336-5.

Want To Learn More From Sharon Hennessey About Hypermobility?
Sharon’s ground-breaking hypermobility educational courses are launching soon – sign up now to know when the courses go live!
Join the wait list to be the first to access exclusive video content, tailored for health professionals, patients, carers, and anyone seeking to better understand hypermobility.
